list of surgeries:
An angiography is a diagnostic procedure that uses X-ray images to look for
blockages or narrow spots in your blood vessels (arteries or veins). An
angiography test can show how blood circulates in blood vessels at specific
locations in your body. Your physician uses an angiography of your heart, neck,
kidneys, legs or other areas to locate the source of an artery or vein issue.
He may want to do an angiography procedure when you have signs of blocked,
damaged or abnormal blood vessels. An angiogram test helps your physician to
determine the source of the problem and the extent of damage to your blood
vessels.
With an angiography procedure, your physician can diagnose and plan treatment
for conditions like:
- Coronary artery disease
- Peripheral artery disease
- Blood clots
- Aneurysm
An angiography procedure involves injecting contrast material (dye) that your
physician can see with an X-ray machine. Images on a screen show blood flow and
blockages in your blood vessels. Your physician will give you medicine to make
sure you’re relaxed and comfortable. Most people receive sedation. Others get
general anesthesia, which makes them sleep. Either way, someone will need to
drive you home afterward.
The day of your angiography
- Do not have breakfast on the day of your procedure.
- Leave your jewelry and other valuables at home.
- Make sure you arrange for a responsible adult to drive you home.
- Bring a current list of your medications and allergies.
- Let the nurse know if you have diabetes.

During an angiography procedure, your physician will:
- Numb the area where the catheter will go.
- Access your blood vessel with a needle.
- Thread a wire through the needle.
- Slide a long, slender tube called a catheter over the needle and into a large
artery (usually in your groin or wrist area).
- Slowly and carefully thread the catheter through your artery until the
catheter’s tip reaches the part of the blood vessel they want to examine.
- Inject a small amount of contrast material (dye) through the catheter and into
your blood vessel segment. For a few seconds, this can make you feel
- Take X-rays.
- Watch where the contrast agent goes on the X-ray monitor to see where and
how well blood is moving in your blood vessels.
How long does an angiography take?
An angiography can take as little as 15 minutes. But some can take a few hours. It
depends on what procedures your physician does after they find the issue.
Angiography is a diagnostic method for vascular artery blockages and is not
known as a treatment method. However, with the passage of time and the
advancement of angiography tools, doctors decided to treat some blockages with
this method in addition to diagnosis, thus the angioplasty method was created.
Angioplasty is a non-surgical method that does not require any special incisions
and is minimally invasive. Angioplasty can perform narrowing and blockages of
vascular arteries as well as repair them, especially in the heart vessels. If the
blockages of the vessels are severe, in some cases the doctor decides to perform
open heart surgery instead of angioplasty or stenting.
This operation, which lasts about 1 hour (angioplasty varies between 0 minutes
and 2 hours but is generally completed within 1 hour). It does not require full
anesthesia and is generally performed with local anesthesia or light anesthesia in
a way that the patient is awake during the operation.
There are some steps that must be taken before the operation, including injecting
some fluids such as sedatives and blood thinners (to reduce blood clotting) such
as anticoagulants into the body with an intravenous catheter, and then the
operation begins.
In angioplasty, the doctor temporarily places a balloon, which is like a small
balloon, in the place where the artery is blocked for a few seconds and inflates it
until the vessel is completely open. After this operation, the vessel opens and
returns to its normal course, but often a spring called a stent is used to prevent
re-blockage.
Of course, placing a spring in a vessel is not such an easy task. In some patients,
after the spring is placed in the vessel, the blood clots so severely that the doctor
has to take the patient back to the angiography room and perform angioplasty.
This sometimes leads to the death of the patient. Adding fluids that thin the blood
is done for this reason.
What is open-heart surgery?
Open-heart surgery helps repair heart defects or damage. In this procedure, the
surgeon removes the breastbone and opens the chest to gain easier access to the
heart.
The most common type of open-heart surgery is coronary artery bypass surgery.
Coronary arteries are responsible for delivering oxygen-rich blood to the heart. If
these arteries become blocked or narrowed, you are at risk for a heart attack. To
prevent this problem, open-heart surgery is performed with a blood vessel graft,
which means that the surgeon takes a healthy blood vessel from another part of the
body and transplants it into the blocked coronary artery. This allows the grafted
vessel to bypass the blocked artery and bring new blood to the heart.
Mitral valve or aortic valve open-heart surgery are also common surgeries that
doctors may recommend. The mitral valve is located between the left atrium and
the left ventricle of the heart and prevents blood from flowing back into the atrium.
The aortic valve is located between the left ventricle and the aorta and prevents
blood from flowing back into the heart after it has been pumped.
In addition, you may need to have open-heart surgery if you have any of the
following conditions:
Arrhythmias, including atrial fibrillation
Congenital heart defects, such as atrial septal defect (a hole in the heart) or
hypoplastic left heart syndrome
Heart failure
Thoracic aortic aneurysm
Open-heart surgery steps; how is the surgery performed?
The length of heart surgery depends on the type of surgery and your individual
needs. For example, coronary artery bypass grafting takes three to six hours. Open-
heart surgery is performed under general anesthesia from start to finish, so you are
asleep during the surgery and do not feel any pain.
After the anesthesia, the surgeon makes a 6- to 8-inch (about 15 to 20 cm) incision
in the middle of your chest and cuts through all or part of your breastbone to gain
access to your heart.
Your medical team may use a cardiopulmonary bypass machine during the
surgery. In this case, your heart stops and the machine takes over the pumping of
your blood. In other words, it circulates your blood throughout your body,
delivering oxygen to it and removing carbon dioxide.
Sometimes, your doctor will perform the surgery without a cardiopulmonary
bypass machine. In this procedure, your heart continues to beat, and a member of
the surgical team uses a device to keep it steady during the procedure.
Abdominal aortic aneurysm surgery
The aorta is one of the largest and most important arteries in the human body,
which is responsible for supplying blood to various parts of the body. The aorta
consists of several parts, the lower part of which is also called the abdominal aorta.
Abdominal aortic aneurysm is a condition in which the abdominal aorta bulges and
is at risk of rupture. The aortic artery may also develop an aneurysm for several
reasons and require treatment. In this article, we will introduce abdominal aortic
aneurysm surgery methods and the importance of performing it.
When does an abdominal aortic aneurysm require treatment?
In most cases, an abdominal aortic aneurysm is diagnosed by chance. In fact, a
specialist may learn about the damage to the abdominal aortic aneurysm during an
examination and imaging to diagnose other diseases. Damage to the aortic
aneurysm usually does not have specific symptoms, which is why a person often
does not know about the existence of this disease. However, some patients may
experience symptoms due to damage to the aortic aneurysm, some of which are:
1. The person is constantly accompanied by abdominal pain.
2. The patient may feel that the abdomen is pulsating like the heart.
3. The patient constantly feels pain in the lower back.
These symptoms are observed when the person only has an abdominal aortic
aneurysm. In some cases, the aortic aneurysm may be accompanied by rupture,
which causes symptoms such as shortness of breath, high heart rate, dizziness,
abdominal pain, back pain, sweating, lethargy and unconsciousness. In such
situations, a cardiologist should be consulted as soon as possible for treatment.
How is abdominal aortic aneurysm treated?
The specialist doctor examines the condition of the abdominal aortic aneurysm
after physically examining the patient and performing tests such as echo,
electrocardiogram, exercise test, imaging, etc. After examining the condition of the
artery; Various methods are used to treat abdominal aortic aneurysm damage, the
most important of which are:
Endovascular aneurysm repair or (EVAR): Endovascular aneurysm repair is
a type of closed surgery that usually does not require an incision in the
abdomen. In fact, after anesthetizing the patient, the surgeon makes a very
small incision in the groin to perform this surgery. Through the incision
made in the groin, the catheter is guided to the aortic aneurysm with the help
of the arteries. At this stage, a relatively small and narrow tube called a stent
is advanced to the aneurysm through the catheter, and the aortic artery is
treated at this point.
Open abdominal aortic aneurysm surgery: In addition to closed surgery, the
condition of the aortic aneurysm in the patient may be such that the
specialist doctor may recommend open surgery to treat the aneurysm. Unlike
EVAR surgery, during this surgery, a relatively large incision is first made
in the abdomen to access the aneurysm. After finding an aortic aneurysm, a
type of artificial tube called a clamp is placed close to the protruding part of
the aorta and the aneurysm problem is completely resolved.
What is the importance of treating an abdominal aortic aneurysm?
Some people may wonder why we should take action to eliminate an abdominal
aortic aneurysm? Unfortunately, those who suffer from an aortic aneurysm in the
abdomen may be exposed to several risks such as aneurysm rupture or disruption
of the blood flow system.
In some cases, the rupture of an aortic aneurysm may be so severe that it causes
bleeding. For this reason, it is better to see a cardiologist as soon as possible to
prevent the growth of an aortic aneurysm, improve the blood flow system, reduce
the symptoms of the disease, and prevent the aneurysm from rupturing.
Tummy Tuck Surgery
A tummy tuck, tummy tuck, or abdominoplasty is a surgical procedure that aims to
improve the shape and elasticity of the abdominal area. This surgical procedure
involves removing excess and sagging fat and skin to improve the shape of the
underlying tissues that support the skin and fat. Tummy tuck surgery can be
performed for cosmetic or reconstructive reasons.
The goal of a tummy tuck is to remove excess skin and fat from the mid and lower
abdomen, as well as to repair muscles that have been separated. It can also help
reduce the protrusion of the abdomen due to excess skin and fat and loose
abdominal muscles.
Although abdominoplasty is considered a cosmetic procedure, it can also have
reconstructive aspects in some cases. Including:
Correction of abdominal deformities caused by pregnancy, obesity and
overweight, severe weight loss, trauma, tumors or other diseases
Correction or relief of structural defects in the abdominal area
Improvement of abdominal muscle function
Restoration of a normal appearance in the abdominal area
Repair of an abdominal hernia that has occurred following previous surgery.
Abdominoplasty
Abdominoplasty is a cosmetic procedure that is very serious and requires rest and
hospitalization for at least one day. This surgery is best performed in equipped
medical centers and hospitals.
It should be noted that the percentage of embolism in this surgery will be higher
than any other surgery and in general, it will be greatly reduced with the necessary
care, but it will never reach zero. Abdominoplasty is most often performed in
conjunction with liposuction of the flanks and stomach area. It will also be
necessary to wear a girdle for three months after surgery.
Abdominoplasty surgery will not be suitable for people whose BMI is high and all
their body parts are facing obesity, because this surgery can remove belly and side
fat, and it will not be suitable for people whose arms, thighs and other body parts
are obese. In such a case, it is better for the patient to first treat and eliminate their
obesity, and then proceed to perform surgery.
Can abdominoplasty surgery be associated with complications and risks?
The surgeries performed today are designed to provide the highest level of safety.
However, there is a possibility of complications. It is worth noting that in any
general anesthesia, there is a risk of risk and pulmonary embolism in any
abdominoplasty, but the probability is negligible if scientific issues are observed
and the facilities of a well-equipped hospital are used. Such as:
Wound infection
Pain and discomfort in the stitches
Hematoma (blood accumulation in the areas around the surgery)
Prominence and clarity of scars
Numbness around the surgical area
Blood clots
Nausea
Abdominoplasty procedure
To perform abdominoplasty, a horizontal incision is made between the pubic
hairline and the navel. The shape and length of the incision depend on the amount
of tissue and fat that needs to be removed. In the next step, the skin is removed and
the underlying abdominal muscles are accessed and repaired.
Another incision is made in the areas around the navel to remove any excess tissue
and fat in the upper abdomen. After the changes are made and the skin and fat are
removed, the remaining skin is sutured and a new hole for the navel is created.
What care is needed after abdominoplasty?
After surgery, a dressing will be placed on the abdomen to protect the
stitches. In addition, the elastic bandage will reduce swelling and
inflammation in the abdomen.
A tube may be temporarily placed under the skin to collect blood and excess
fluid.
A special garment that is provided to the patient must be worn for six weeks
to prevent fluid accumulation and protect the abdomen.
For several weeks after surgery, strenuous physical activities that put
pressure on the abdomen and stitches should be avoided.
What is a cholecystectomy?
A cholecystectomy is surgery to remove your gallbladder. The gallbladder is a
small organ located under your liver. It is located on the upper right side of your
abdomen or stomach. The gallbladder stores a digestive juice called bile that is
made in the liver.
There are 2 types of gallbladder removal surgery:
Open (traditional) procedure. In this procedure, 1 incision (cut) about 4 to
6 inches long is made in the upper right side of your abdomen. The surgeon
finds the gallbladder and removes it through the incision.
Laparoscopic procedure. This procedure uses 3 to 4 very small incisions. It
uses a long, thin tube called a laparoscope. This tube has a small video
camera and surgical tools. The tube, camera, and tools are inserted through
the incisions. The surgeon performs the surgery while watching a TV
monitor. The gallbladder is removed through 1 incision.
Laparoscopic cholecystectomy is less invasive. It uses very small incisions in your
abdomen. There is less bleeding. Recovery time is usually shorter than open
surgery.
In some cases, the laparoscope may show that your gallbladder is very diseased. Or
it may show other problems. Then the surgeon may have to use an open surgical
procedure to safely remove the gallbladder.
What are the risks of a cholecystectomy?
Some possible complications of a cholecystectomy may include:
Bleeding
Infection
Damage to the tube (bile duct) that carries bile from the gallbladder to the
small intestine.
Liver damage
Scarring and numbness at the incision site
Protrusion of an organ or tissue (hernia) at the incision site
During a laparoscopic procedure, surgical instruments are placed in your abdomen.
This may damage your intestines or blood vessels.
You may have other risks that are specific to you. Be sure to discuss any concerns
with your healthcare provider before the procedure.
What happens during a cholecystectomy?
You may have a cholecystectomy as an outpatient or as part of your hospital stay.
The way the surgery is performed may vary depending on your condition and the
performance of your healthcare provider.
A cholecystectomy is usually performed while you are given medication to put you
in a deep sleep.
In general, a cholecystectomy follows this process:
You will be asked to remove any jewelry or objects that may interfere with
the surgery.
You will be asked to undress and given a gown to wear.
An intravenous (IV) line will be placed in your arm or hand.
You will lie on your back on the operating table. Anesthesia will be initiated.
A tube will be placed in your throat to help you breathe. The
anesthesiologist will monitor your heart rate, blood pressure, breathing, and
blood oxygen levels during surgery.
If there is a lot of hair at the surgical site, it may be clipped.
The skin over the surgical site will be cleaned with a sterile solution
(antiseptic).
Open cholecystectomy
An incision will be made. This incision may be angled under your ribs on the right
side of your abdomen. Or it may be made in the upper part of your abdomen.
Your gallbladder will be removed.
In some cases, 1 or more drains may be placed in the incision. This allows fluid or
pus to drain.
Laparoscopic cholecystectomy
About 3 or 4 small incisions will be made in your abdomen. Carbon dioxide gas is
injected into your abdomen to inflate it. This allows the gallbladder and nearby
organs to be seen more easily.
A laparoscope is inserted into one incision. Surgical instruments are inserted
through other incisions to remove the gallbladder.
After the surgery, the laparoscope and instruments are removed. Carbon dioxide
gas is released through the incisions. Most of it will be reabsorbed by your body.
Completion of the procedure, both methods
The gallbladder is sent to a laboratory for testing
The incisions are closed with stitches or surgical staples
A sterile bandage or dressing or adhesive tape is used to cover the wounds
Colorectal Surgery
Colorectal surgery is a branch of medicine and surgery that deals with conditions
of the large intestine. Colorectal means that the large intestine and rectum are
affected by the techniques of this surgical procedure. The colon is called the
middle part of the intestine. The rectum is also considered the last part of the colon.
The rectum is anatomically directed directly to the outside of the body.
What conditions does colorectal surgery treat?
Common diseases of the digestive tract, as well as less common ones, can occur
for a variety of reasons. These conditions also have their own characteristics and
symptoms. Colorectal surgery is mainly used to treat benign digestive tract
conditions such as diverticulosis, ischemic colitis, and long-term inflammatory
bowel diseases such as Crohn's and ulcerative colitis.
The second use and role of colorectal surgery is to treat malignant digestive tract
conditions. Among the malignant diseases treated with this surgery is colorectal
carcinoma. Although colon polyps are often benign growths that have grown out of
the intestinal mucosa, it is possible that colon adenomas can sometimes be
identified as precursors to colon cancer.
Hereditary syndromes can also occur that are associated with colon polyps and an
increased risk of cancer. Familial adenomatous polyposis is one of the hereditary
conditions of the digestive tract. Another benefit of colorectal surgery is the
treatment of abnormalities and injuries of the digestive tract. Colorectal surgery is
also effective in treating anal canal conditions. Anal canal conditions are injuries
that occur in the excretory tract of the digestive tract.
What treatment options are available to colon surgeons?
When choosing a surgical method for treating a gastrointestinal condition in the
colon and rectum, doctors consider whether the condition is malignant or just a
benign condition. They also consider whether they can temporarily or permanently
preserve and treat the bowel. Sometimes, the surgeon will prescribe an artificial
bowel outlet for treatment or simply to treat and relieve the condition.
There are also less invasive, non-surgical treatment options, as well as endoscopic
procedures that are performed only through the bowel. Sometimes, the surgeon
will use laparoscopic techniques, open surgery, and other combined forms of
treatment. The success of the treatment and recovery of the bowel after surgery
also depends on the blood supply to the intestinal tract and the drainage of the
lymph nodes. But more importantly, the treatment and its level of effectiveness
depend mainly on the type of condition and its severity.
What is the purpose of colorectal surgery?
According to the primomedico website, as the name suggests, this invasive
treatment method is used to remove the colon or parts of it. Colorectal surgery is
also the best treatment and surgery for gastrointestinal disorders in the posterior
and posterior parts.
Colorectal surgery involves examination, diagnosis, and consideration of
appropriate treatment options, such as non-surgical treatments instead of surgical
treatment. Finally, this treatment method ends with post-operative care or, in other
words, is completed.
Why should I have colorectal surgery?
Many people with rectal, anal, and colon problems believe that they can overcome
the disease without surgery, or that surgery cannot improve their condition. If the
tumor is very large or if it is worse and has spread beyond the intestinal wall, the
doctor will determine that surgery is the best way to deal with the disease and
destroy it.
Rest assured that today in the field of colorectal surgery, there are new and
effective techniques that doctors can use to eliminate all symptoms of colorectal
cancer and other conditions in this area of the digestive tract. Also, with timely and
proper treatment, the risk of recurrence and progression of the disease is
minimized.
Types of Advanced Colorectal Surgery
Laparoscopic Colon Resection
In this colorectal surgery method, doctors make a very small incision to remove the
tumor. In this surgery, the surgeon may also remove lymph nodes at risk of being
affected by the condition, depending on the diagnosis.
Rectal Cancer Surgery
When cancer is diagnosed in the last 20 centimeters of the colon, it is called rectal
cancer. In rectal cancer surgery, the surgeon removes the fatty tissue around the
tumor using advanced techniques. This method is more invasive and helps
surgeons access all affected lymph nodes. This surgery greatly reduces the risk of
cancer recurrence.
Advanced Robotic Technology
As the name suggests, this surgical procedure uses a robotic surgical system to
treat the condition. The doctor treats the condition by guiding and controlling the
robot during the surgery. This surgical procedure is usually very useful when the
area affected by the condition is difficult to access. This invasive and advanced
surgery can also have a significant impact on reducing the risk of recurrence and
progression of the disease.
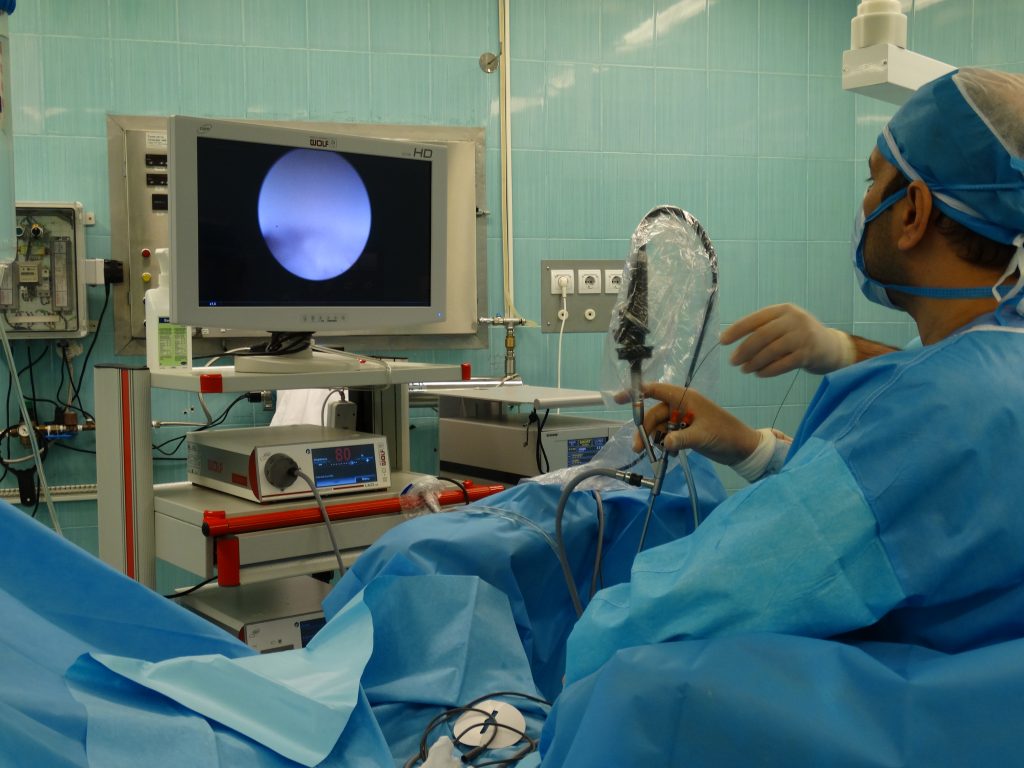
What is cystoscopy?
Cystoscopy is a combination of cysto and scopy. Scopy means to examine with a
camera and cysto means bladder. So, the literal meaning of this procedure is to
look into the bladder with a camera. Urologists use cystoscopy to diagnose
problems in the urinary tract. A cystoscope is a thin tube with a camera and light at
the end. During a cystoscopy, the doctor inserts the tube through the urethra into
the bladder so that he can see the inside of your bladder. The magnified images
from the camera are displayed on a screen for the doctor to see.
Who needs a cystoscopy?
A urologist may recommend a cystoscopy if you experience the following:
Bladder control problems such as urinary retention (inability to completely
empty your bladder) or incontinence (inability to control the flow of urine)
Pain during urination
Painful urination (dysuria)
Blood in the urine
Bladder stones
Recurrent urinary tract infections (UTIs)
People with cancerous or noncancerous tumors
What conditions is a cystoscopy used to diagnose?
Conditions diagnosed with cystoscopy include: Bladder stones and bladder
inflammation Enlarged prostate (benign prostatic hyperplasia) Bladder cancer or
cancer of the urethra Bladder control problems Urethral strictures and urinary
fistulas Diagnosis and sampling of small tumors Cystoscopy Uses of cystoscopy
for treatment How cystoscopy is performed For this test, you will need to remove
all or most of your clothing and wear a cloth covering. About half an hour before
the test, you will be given a sedative to help you feel more comfortable during the
test. An intravenous (IV) needle may also be placed in a vein in your arm so that
medications and fluids can be given to you. You will lie on your back on a bed
with your knees bent and your legs spread apart. Your legs or groin may be bound
with special stirrups. Your genital area will be cleaned with a disinfectant solution,
and a sterile cloth will be wrapped around your navel and groin.
Postoperative care after cystoscopy
It is normal to experience burning sensation when urinating, blood in the
urine, and mild pain after a cystoscopy and will subside with fluids. It is best
to avoid foods that stimulate the bladder while the burning sensation
persists.
Using a warm bath, placing a warm, damp towel on the urethra and external
genitalia, and taking a warm shower can also help reduce pain and
subsequent complications of cystoscopy.
Due to the manipulation of the urinary system and the relaxation of the
muscles caused by the injection of anesthetics, a person may experience
difficulty urinating or even urinary retention.
This procedure is usually performed without the need for general anesthesia
and with local anesthesia. After the cystoscopy, the patient gets out of bed,
puts on his normal clothes, and is discharged after 1-2 hours of observation.
It is recommended to have someone with you. Performing a normal
cystoscopy usually does not have any special complications, and the person
can continue his normal life (after the anesthetic drugs have taken effect and
he has fully regained consciousness).
In rare cases, performing a cystoscopy can cause urinary tract infection or
even testicular infection. In case of fever and chills, or if the above problems
continue, or if bleeding and burning sensation in the bladder do not resolve,
contact your doctor after 2 to 3 days.
Arteriovenous fistula creation
Arteriovenous fistula creation is a surgical procedure performed by a vascular
surgeon to create a connection between an artery and a vein.
The fistula is usually located on the forearm or upper arm. However, it may also be
located on the leg. Creating an AV fistula increases the pressure and blood flow in
the vein, causing the vein to become larger and stronger. The enlarged vein
provides easy and reliable vascular access for hemodialysis treatments. Indications
for Arteriovenous fistula creation: An arteriovenous fistula may be created for
dialysis in kidney patients.
Preparing for an arteriovenous fistula creation
In preparation for creating an arteriovenous fistula, a Doppler ultrasound is
performed to map the blood vessels. The ultrasound shows the speed of blood flow
through the various blood vessels in the area and enables your surgeon to select the
most appropriate blood vessel for creating the fistula.
You should tell your doctor about any allergies and medications you take regularly,
as some medications, such as blood thinners, may need to be temporarily stopped a
week before surgery. You may be asked to refrain from eating or drinking after
midnight the day before surgery.

Procedure for creating an arteriovenous fistula
Creating an arteriovenous fistula involves the following steps: The skin over the
AV fistula site is cleaned with an antiseptic solution, and a local anesthetic is
applied to numb the area.
In another procedure, general anesthesia may be used so that you are asleep during
the procedure. With local anesthesia, you will remain awake and may feel pressure
at the site, but you will not feel any pain.
A small incision is made to access the blood vessels. The selected artery and vein
are cut and surgically connected with stitches. The skin incision is then closed with
stitches, and a bandage is placed over the incision.
Recovery and Postoperative Care for Arteriovenous Fistula Creation
AV fistula creation can be done in an outpatient setting, and most patients can be
discharged after a few hours of recovery.
There may be mild discharge from the incision site for up to 24 hours and some
pain for a few days after surgery. You will be given medication for any post-
operative pain, and you will be advised to keep your arm elevated to reduce
swelling.
You will be given specific instructions on how to care for your AV fistula access
site. It will take about 2 to 3 months for the fistula to grow and mature enough to
be used for hemodialysis.
You should take the following precautions to protect your fistula site:
Wash the vascular access site every day and keep it clean and dry.
Make sure your doctor examines the fistula site before each dialysis session.
Use the fistula site only for dialysis. Be careful not to hit or damage the
fistula site.
Check for a rhythmic vibration at the fistula site, which indicates that the
AV fistula is healthy.
Avoid placing a blood pressure cuff, tight clothing, or jewelry over the
fistula site.
Do not lift heavy objects with the arm that has the fistula.
Avoid sleeping on the arm that has the fistula.
Do not place your arm under your head or body.
Report any signs of infection, such as redness, swelling, or pus discharge, to
your doctor as soon as possible.
Risks and complications of AV fistula
Creating an AV fistula is a safe procedure. However, as with any surgery, there are
risks and complications that may include:
Excessive bleeding
Infection
Swelling
Pain
Clot formation that may narrow or block the AV fistula
Benefits of an arteriovenous fistula
Some of the benefits of an AV fistula (Arteriovenous fistula) in the treatment of
end-stage renal failure include:
Can be used for a longer period of time compared to other types of vascular
access
No need to place a foreign substance in the body
Optimizes blood flow for effective hemodialysis while minimizing treatment
time
Reduces the risk of infection
Faster recovery and faster return to daily activities
Discectomy is a surgical option used in the case of a herniated disc. This approach
involves removing more or less of the affected intervertebral disc. Discectomy is
generally used when patients are resistant to conservative treatments (medications
or physiotherapy) or when patients experience more severe symptoms (back pain,
loss of sensation, difficulty walking, etc.). From a practical point of view, the
surgeon, under general anesthesia, removes the herniated disc fragment using more
or less invasive techniques to allow the patient to recover quickly. If it is necessary
to remove a large portion of the nucleus pulposus, discectomy is accompanied by
the placement of a prosthesis (or a spacer made of artificial or autologous bone)
between the two affected vertebrae.
Discectomy
What is a herniated disc?
A herniated disc is a relatively common spinal condition that can also affect young
people. The most affected age group is between 30 and 50 years. The nucleus
pulposus is made of spongy tissue, located in the center of the intervertebral disc,
and is held in place by a cartilaginous covering (annulus fibrosus). It also holds the
intervertebral disc together with its two vertebrae.
The annulus fibrosus can deform or rupture under the elastic pressure of the
nucleus pulposus (herniated disc), causing the nucleus to escape (extruded disc)
and invade an unrelated space in the vertebral canal (herniated disc migration). In
these cases, the nucleus pulposus comes into contact with nerve roots, irritating
them physically and chemically. These symptoms are commonly associated with a
herniated disc.
What causes a herniated disc?
A herniated disc is the result of certain stresses that wear down the annulus
fibrosus that is placed to protect the nucleus pulposus. Sometimes, intervertebral
discs can become overstretched due to strenuous work or severe trauma to the
spine during sports, weightlifting, or habitually sitting in awkward positions. This
disorder can also be a direct consequence of aging-related degenerative processes
in the bone structures of the spine. Herniated discs mainly affect the cervical,
thoracic, and lumbosacral spine.
Signs and Symptoms of a Herniated Disc?
A herniated disc can be very debilitating. The nucleus pulposus of an intervertebral
disc that protrudes from the annulus fibrosus can compress the nerve roots exiting
the spinal canal, causing severe pain that can also limit normal movement. These
symptoms can affect the neck or back or can spread to the arms or legs. In the
initial stage, which is characterized by symptoms of irritation of the nerve
structures, there are sensory and motor deficits. Therefore, numbness or weakness,
motor problems, loss of muscle strength, numbness and tingling in the limbs may
occur.
What is a discectomy?
Discectomy is a surgical procedure used to remove the damaged part of the
intervertebral disc affected by a herniated disc. Discectomy is used when there is a
significant decrease in strength or the pain increases despite the use of medication
and physiotherapy.
How is a discectomy performed?
There are two common methods of intervention in the case of a herniated disc,
traditional microdiscectomy and endoscopic microdiscectomy. Below I have
reviewed the performance of their methods:
Traditional microdiscectomy
Microdiscectomy is a percutaneous technique that guarantees good results. In
practice, it consists of removing the herniated material and the disc that protrudes
from it. This technique is quite similar to discectomy.
Endoscopic microdiscectomy
This procedure uses an endoscope, an instrument consisting of a very small
flexible tube, formed by a series of very thin optical fibers connected to a
microcamera. After making an incision of a few millimeters, the endoscope is
inserted into the area to be treated by penetrating the disc laterally. It is precisely
through these small instruments that the surgeon removes the herniation. Both of
these procedures are performed under general or spinal anesthesia.
Laser discectomy
This procedure uses a laser beam that is applied directly to the nucleus of the disc,
which removes the herniation through special cannulas. This procedure can be
performed under radiological control and through a percutaneous procedure. This
procedure may make treatment of lumbosacral disc herniation more difficult.
Disc Coblation
This minimally invasive procedure involves inserting a needle into the disc space,
under radiological control, to which an electrode is applied. Through the
transmission of high-frequency energy (radiofrequency), it is able to destroy part
of the nucleus pulposus. As a result, the shrunken disc no longer compresses the
nerves, so the pain disappears and mobility improves. This type of treatment is
indicated (priority) in the early stages of herniation.
Weight loss surgery is a series of surgical procedures aimed at weight loss. Like
other weight loss surgeries, gastric sleeve surgery is suitable for those who, for
whatever reason, diet and exercise have not been successful in losing weight. In
gastric sleeve surgery, a gastroenterologist removes a large portion of the stomach
and reshapes the stomach to resemble a small banana or sleeve. The removed parts
of the stomach are the parts that produce the hunger hormone, ghrelin.
This procedure is newer than gastric bypass surgery and is usually less expensive
than bypass surgery. Various studies have shown that sleeve surgery is as effective
as gastric bypass surgery. When you see a gastroenterologist, your doctor will
review your conditions and wishes and, based on your physical condition and
health, will recommend gastric sleeve surgery if appropriate.
What is a gastric sleeve or sleeve gastrectomy?
What is a gastric sleeve? Gastric sleeve surgery is a type of weight loss surgery in
which a large part of the stomach is removed. Gastric sleeve surgery is a restrictive
surgery in which about 75% of the stomach volume is removed; as a result, the
person feels full after eating a small amount of food. This surgical option does not
change the intestinal tract.
This surgery also makes the person feel less hungry because a smaller stomach
secretes lower levels of the hormone ghrelin (which leads to hunger); as a result,
the person will experience long-term appetite suppression.
Although sleeve gastrectomy leads to significant weight loss, it is also associated
with certain risks and side effects. Therefore, before deciding to undergo this
procedure, consult a gastroenterologist and only undergo gastric sleeve surgery
when the benefits of this procedure outweigh the risks.
What are the steps of gastric sleeve surgery?
The gastric sleeve procedure involves a series of steps, which are outlined below:
• Laparoscopic gastric sleeve surgery (also known as closed surgery or LSG)
requires general anesthesia in a hospital setting and is performed by a
gastroenterologist through approximately five small incisions in the patient’s
abdomen.
• The surgeon performs the procedure using a long, thin telescope with a small
camera at the end. This instrument is used to remove about 80% of the stomach.
• The abdomen is inflated by injecting carbon dioxide gas into the abdomen. A
special instrument called a trocar is then used to enter the abdomen. First, a
silicone tube is passed from the mouth to the outlet of the stomach to adjust the
width of the remaining stomach and separate it from the fatty tissue surrounding
the stomach, nearby vessels, and spleen. The excess stomach is then cut and
removed with a special device called a stapler. After the gastrectomy, about 80 to
150 mm of the stomach volume remains.
• The removed part is removed from the abdomen and sent to the pathology
department for examination. Then, the bleeding at the incision site and the stapled
part is controlled. Additional metal clips or several stitches can be used.
• Also, if necessary, some special medications are placed on the wound to stop the
bleeding. Then, a silicone drain is placed in the surgical area to drain the
accumulated fluids. Finally, the wound is closed and the surgery is completed.
What is the aftercare after gastric sleeve surgery?
If you have had gastric sleeve surgery, you should first start with liquid foods.
After a few weeks, you can eat pureed foods and finally solid foods. During this
time, you will notice that your meal consumption will be much less than before and
you may have to avoid drinking liquids with meals due to the shrinking of the
stomach.
The proper functioning of the hip joint depends on various factors, including:
tendons, muscles, ligaments, and bones. If these organs are in harmony with each
other, a person will have no problems when walking. There are many factors that
can be the main causes of pain in the hip joint, which are:
Among the most important causes of hip joint destruction and wear and tear is
osteoarthritis. This disease is seen in the majority of people at any age and its
likelihood of occurring increases with age. Femoral head necrosis or blackening of
the bone head, which causes premature wear and tear. This condition is seen in
young or middle-aged people. The occurrence of this disease is seen in people who
use corticosteroids. Deformation of the acetabulum cavity, which is a type of
acetabular dysplasia, this disease can cause joint destruction and wear and may
occur between the ages of 30 and 50. Congenital dislocation of the hip joint is one
of the factors that causes arthritis in a person. Early osteoarthritis causes include
impingement of the femoral head and acetabulum socket. Due to the failure of the
acetabulum fractures to heal properly, joint destruction and wear can be expected.
If a person has one of the types of rheumatism, rheumatoid arthritis or ankylosing
spondylitis, they should have periodic checkups to prevent hip joint destruction.
How to perform hip joint surgery
The anatomy of the hip joint consists of two bones next to each other. Thus, in the
upper part of the hip joint structure, the acetabulum socket, which is in the shape of
a hemisphere, is located and this socket is part of the pelvis. In the upper part of the
hip joint, the femoral head is located, which is spherically located inside the
acetabulum socket.
When an orthopedic surgeon performs surgery, he uses a special planer to scrape
the inside of the acetabulum cavity to remove the remaining cartilage and excess
bone that has been worn away from the head of the bone and shape it into a perfect
hemisphere. In the femoral head area, the orthopedic surgeon completely removes
the head of the bone from the patient's body.
Next, the surgeon cuts the femoral neck, which is located between the femoral
head and the femoral shaft, using special orthopedic saws. After this cut is made,
the femoral head is completely removed.
In the next step, the orthopedic surgeon places a metal or plastic cup in the
acetabulum cavity and places a metal head in the femoral neck area. Finally, after
preparing both parts, they are placed inside each other. After placement, the joint
movement is checked to ensure that the artificial hip joint is properly in place.
Who is suitable for hip replacement?
Surgery can be helpful for people who have pain and limited mobility in the hip
area, and some people also have short legs, in which case hip replacement surgery
can be effective to some extent.
Hip replacement or hip arthroplasty is one of the methods that has been helpful in
recent years for people who need hip replacement due to joint damage caused by
diseases such as arthritis or various injuries that may occur in daily life, and it
increases the recovery process of people.
Hip replacement surgery is one of the best treatment methods for long-term
improvement of the hip for people who have not received results from other
treatment methods. By performing this surgery, pain in the hip joint can be
completely eliminated and a pain-free life can be experienced.
Post-surgery care for hip replacement
After surgery, the patient usually complains of pain, which will be relieved
by painkillers.
The patient may have shortness of breath at first, which could be due to the
anesthesia and the medications injected.
But what is important is that the patient should cough and take deep breaths
to clear the lungs.
It is recommended to avoid taking blood thinners to prevent blood clots.
The day after hip replacement
Now it is time for the patient to walk with the new joint. Physiotherapy exercises
help strengthen muscle strength and improve range of motion. The patient is asked
to get up, hold the sides of the bed, and slowly start walking.
One to two days after hip replacement surgery
At this stage, the patient is able to do more physical exercises and can walk with
the help of a cane or walker. The diet can also continue as before. Note that it is
recommended that the patient have a liquid diet on the first day.
Two to three days after hip replacement surgery
If there are no special problems and the patient is able to walk, he will be
discharged, but note that driving will be prohibited for three to six weeks.
The fourth day after hip replacement surgery
The stitches should be taken care of, the stitches should not be wet under any
circumstances or creams and ointments should be applied to them.
To relieve pain, an ice compress can be used for ten to fifteen minutes, several
times a day.
What is knee replacement surgery?
Knee replacement surgery, or arthroplasty, is performed to relieve pain and
improve the function of the knee joint. In this surgery, the damaged joints,
including the thigh bone, kneecap, and shin bone, are removed and replaced with
artificial joints (prostheses). Prostheses can be made of metal, ceramic, or heavy
plastic. Arthroplasty can be performed on many joints in the body, including the
shoulder, elbow, and ankle. However, it is most commonly performed to replace
the knee and hip joints. A doctor may recommend this surgery when other
treatments have not worked and a person may have lost the ability to move their
joints.
How to perform knee replacement surgery
This surgery is very sensitive and must be performed in a hospital. For knee
replacement surgery, the person must be anesthetized. Sometimes the surgeon may
use spinal anesthesia. During this surgery, the following steps are taken.
• You will need to change into an operating room gown.
• A vein in your arm will need to be prepared for the injections during the surgery.
• Sometimes a urinary catheter will be placed for the patient.
• If there is excess hair at the surgical site, it will be shaved before the procedure
begins.
• The skin at the surgical site will be cleaned with antiseptic.
• An incision will be made in the joint area.
• The damaged parts of the joint will be corrected as much as possible and removed
if necessary.
• Prostheses will be placed in the place of the previous joints.
• The incisions will be sutured.
• A sterile bandage or dressing will be placed over the sutures.
• In knee replacement surgery, an incision will be made in the knee and a
prosthesis will be inserted to replace the damaged joint.
• In knee replacement surgery, an incision is made on the knee and a prosthesis is
inserted to replace the damaged joint.
Postoperative care for knee replacement
• You will stay in the recovery room for 2 hours after your arthroplasty surgery.
Some people are discharged the same day, while others will need to stay in the
hospital. After the surgery, you should gradually try to move your foot and ankle.
This will help increase blood flow to the leg muscles.
• Your doctor may prescribe blood thinners to reduce the risk of blood clots
forming at the surgical site. Painkillers may also be prescribed to reduce pain.
• Your physical therapist will teach you exercises to do after the surgery. Do the
exercises regularly and follow a healthy diet.
• The surgical area should be kept clean and dry. Your doctor will give you
specific instructions for bathing. The stitches will be removed a few weeks after
the surgery.
• You will not be able to do your usual activities for a few weeks. For this reason,
you should check the following at home and purchase the necessary equipment.
• Proper railings on stairs
• Bathroom safety
• Toilet
• Bath seat and shower hose
• Firm cushion when sitting
Laminectomy Surgery
Back or neck pain that interferes with normal daily activities may require surgery
to treat. A laminectomy is a type of surgery in which a surgeon removes part or all
of the lamina of a vertebra in the spine. This helps relieve pressure on the spinal
cord or nerve roots that may be caused by injury, a herniated disc, a narrowing of
the spinal canal (spinal stenosis), or a tumor. A laminectomy is only considered if
other medical treatments have not worked.
Back or neck pain can range from mild, dull, and annoying to constant, severe, and
debilitating. Pain in the spine can limit a person’s ability to move and function. A
laminectomy may be done to relieve pressure on the spinal nerves, treat a disc
problem, or remove a tumor from the spine.
One of the most common reasons for a laminectomy is a herniated disc in the
spine.

A disc can become displaced or damaged due to injury or a ruptured disc. When
the disc presses on the spinal nerves, it causes pain, and sometimes numbness or
weakness. The numbness or weakness is felt in the part of the body where the
nerve is involved, often the arms or legs. The most common symptom of a
herniated disc is sciatica. This is a sharp, shooting pain along the sciatic nerve that
spreads from the buttock to the thigh and down the leg.
If other medical treatments are not effective, surgery may be an option. Some
medical treatments for pain may include:
Changes in activity
Medications such as muscle relaxants, anti-inflammatory drugs, and
painkillers
Spinal injections
Physical rehabilitation, physical therapy, or both
Occupational therapy
Weight loss (if overweight)
Quitting smoking
Assistive devices, such as a back brace
Laminectomy is usually done for back pain or neck pain that persists after medical
treatment. Or it is done when the pain is accompanied by symptoms of nerve
damage, such as numbness or weakness in the arms or legs. Loss of bowel or
bladder control due to pressure in the neck or lower spine also usually requires
surgery.
What happens during a laminectomy?
A laminectomy usually requires a hospital stay. The procedures may vary
depending on your condition and the doctor's procedures.
A laminectomy may be performed while you are asleep under general anesthesia.
Or it may be done while you are awake under spinal anesthesia. If spinal anesthesia
is used, you will have no sensation from your lower back down. Newer techniques
are being developed that may allow laminectomy to be performed under local
anesthesia on an outpatient basis. Your doctor will discuss this with you.
In general, a laminectomy procedure follows this procedure:
You will be asked to wear a gown.
An IV (intravenous) line may be placed in your arm or hand.
Once you are under anesthesia, a urinary drainage catheter may be placed.
If the surgical site is covered with excess hair, the hair may be removed.
You will lie on your side or stomach on the operating table.
The anesthesiologist will continuously monitor your heart rate, blood
pressure, breathing, and blood oxygen levels during surgery.
Healthcare workers will clean the surgical site with a skin antiseptic
solution.
The surgeon will make an incision over the selected vertebra.
The surgeon will separate the muscles.
The surgeon will remove the bony arch at the back of the vertebra (the
lamina) to relieve pressure on the nerves in the area. This may include
removing a bone spur or tumor, or removing all or part of a disc.
In some cases, spinal fusion may be done at the same time. During spinal
fusion, the surgeon joins 2 or more bones in your spine.
The incision will be closed with stitches or surgical staples.
What is PCNL?
This procedure is usually performed under general anesthesia. During the
procedure, a thin tube (catheter) is inserted into the bladder. This catheter is held in
place with a balloon and drains urine from the bladder.
After the catheter is placed in the bladder, another catheter may be inserted into the
ureter (ureter). To better see the exact location of the stone, a contrast agent (dye)
is injected through this catheter. This dye helps us to image the urinary system
better during the procedure using radiology or ultrasound and to have easier access
to the kidney to remove the stone.
PCNL Procedure
Once the exact location of the stone is determined, we use a very fine needle to
access the urine collecting system in the kidney and then insert a guidewire to
create a safe path for the nephroscope to enter. A nephroscope is a tube-shaped
instrument used to look directly into the kidney.
The access path is carefully opened to allow the nephroscope to be inserted.
Some stones can be removed directly using a grasping instrument. This procedure
is called a nephrolithotomy. Larger stones may also need to be broken up with a
device such as a laser, also called a nephrolithotripsy.
After all the stones are removed, the surgeon uses a contrast agent to make sure
that no stones or fragments of them remain in the kidney. Easy movement of the
contrast agent from the bladder shows that there are no stones in the ureter.
In some patients, a small temporary tube called a Double-J may be placed to make
sure that swelling does not block the flow of urine. This catheter remains in place
in both the kidney and bladder due to its J-shaped bend. At the end of the
procedure, a urinary catheter may also be attached.
Preparations for PCNL
To best prepare for PCNL, consider the following points and remember that your
doctor's instructions take priority. Some important points that your doctor may
mention include:
When to stop taking certain medications, such as blood thinners
A specific time to empty your bladder before surgery
Planning for pain medication after surgery
Coordinating with a companion to return home after surgery
Abstaining from eating, drinking, or smoking for about 6 to 8 hours before
surgery (to prepare for anesthesia)
The anesthesiologist will select the appropriate anesthesia method.
Preparations for PCNL
Having your companions (partner, relatives, or friends) read information about
PCNL can help you feel more relaxed and prepared. Write down your questions so
you don’t forget important points when you meet with your doctor or nurse. Have a
loved one accompany you during your visit to help remind you of any questions
you missed.
What to expect after PCNL surgery?
After surgery, you will be taken to the recovery room or your room, depending on
your hospital. Nurses will regularly check your blood pressure, heart rate, and pain
level. Also, be sure to ask your nurse about your hospital visit times.
JJ stent:
In some cases, a small temporary tube called a double-J stent may be placed in the
ureter to help urine flow to the bladder. This is done when the ureter is expected to
swell slightly after surgery. The JJ stent can be removed before you leave the
hospital or shortly thereafter, in a separate appointment with your doctor.
Urinary catheter:
You may also have a urinary catheter inserted after surgery. This tube is inserted
through your urethra into your bladder and helps urine flow more easily. You will
also be given fluids to help you stay hydrated. The urinary catheter is usually
removed shortly after surgery (within a few days).
Nephrostomy tube:
In some cases, a tube called a nephrostomy tube may be placed in your kidney
during surgery. If needed, this tube will remain in place for a short time (possibly
after you leave the hospital). The nephrostomy tube comes out of the incision in
your skin and directs blood and urine from the surgery directly from your kidney
into a special drainage bag. This tube is usually removed a few days after surgery.
After PCNL
You will be discharged within a few days of your surgery if you are able to empty
your bladder well and do not have a fever or severe pain. You may also experience
mild to moderate pain in your lower abdomen and a constant need to urinate. These
symptoms are usually due to the presence of a JJ catheter or stent and are not a
cause for concern. Your doctor will prescribe medication to control this pain, so be
sure to talk to your nurse or doctor if you experience any pain.
What causes urinary tract stones?
Urinary tract stones are hard deposits of minerals and salts that form inside the
kidneys of an affected person. Several factors contribute to the formation of these
types of stones, including poor diet, being overweight, inactivity, certain medical
conditions, and taking certain supplements and medications.
Kidney, ureter, and bladder stones can affect any part of your urinary tract, from
the kidneys to the bladder. Stones form when urine becomes concentrated,
allowing the minerals to crystallize and stick together, forming kidney, ureter, or
bladder stones.
Risk factors for developing urinary tract stones
Factors that increase your risk of developing urinary tract stones include the
following:
Family or personal history: If someone in your family has had urinary tract
stones, you are more likely to develop urinary tract stones than other people.
If you have had one or more cases of urinary tract stones in the past, you are
at risk for developing urinary tract stones.
Risk factors for developing urinary tract stones
Dehydration: Not drinking enough water during the day can increase your
risk of developing urinary tract stones. People who live in hot, dry climates
and those who sweat a lot may be at a higher risk of developing urinary tract
stones than others.
Special diets: A diet high in protein, sodium (salt), and sugar may increase
your risk of developing some types of urinary tract stones. This is especially
true for a high-sodium diet. Too much salt in the diet increases the amount
of calcium that the kidneys have to filter, significantly increasing the risk of
developing urinary tract stones.
Dietary risk factors for urinary tract stones
Obesity: A high body mass index (BMI), large waist size, and weight gain
are associated with an increased risk of developing urinary tract stones.
Dietary diseases and surgery: Gastric bypass surgery, inflammatory bowel
disease, or chronic diarrhea can cause changes in the anatomy and processes
of the digestive tract that affect calcium and water absorption, increasing the
amount of stone-forming materials in the urine and increasing the likelihood
of developing urinary tract stones.
Other diseases, such as renal tubular acidosis, cystinuria, hyperparathyroidism, and
recurrent urinary tract infections, can also increase the risk of developing urinary
tract stones.
Some supplements and medications, such as vitamin C, dietary supplements,
laxatives (if taken in excess), calcium-based antacids, and certain medications used
to treat migraines or depression, can increase your risk of developing urinary tract
stones.
What is TUL?
A TUL is a common procedure for treating the worst types of kidney, ureter, and
bladder stones, in which the stone can be removed through a special telescope, or
in special cases, a laser can be used to break the stone into very small pieces.
What is TUL?
A TUL is performed under general anesthesia or in an operating room under
general anesthesia. Depending on the stone and your anatomy, a TUL can take
anywhere from 30 minutes to 2 hours and can be very simple or quite complex.
In a TUL, your doctor will first look inside your bladder and insert a special
guidewire into your ureter. X-rays may be done before the actual procedure to
locate the stone, and this is done with the help of real-time X-rays (called
fluoroscopy).
Depending on the location of the stone, a shorter, semi-rigid scope or a longer,
flexible ureteroscope is inserted into the ureter until the stone is found. Sometimes
during a TUL procedure, the ureter must be dilated with a special balloon so that
the scope can be inserted.
A ureteroscope is a special, very thin instrument used to directly view and
visualize the inside of the ureter. Some ureteroscopes are like a very long, flexible
straw. Other types of ureteroscopes are more rigid and sturdy. Overall, a large
number of procedures are performed each year using a ureteroscope.
What is TUL aftercare?
After the TUL procedure, to achieve the best results, some care is needed, which
we will introduce and review in detail below:
After the TUL procedure, ask someone to drive you home from the hospital.
Once you get home, you will need to rest.
Most people can return to their normal daily activities after the TUL
procedure after 1 or 2 days of recovery and the necessary aftercare after the
TUL procedure.
In the weeks following the TUL procedure, drink plenty of water. This will
help pass any remaining stone fragments. In this case, your doctor or
surgeon may give you a medication called an alpha blocker to make it easier
for stone fragments to pass through your urinary tract.

